Expectant parents often feel a mix of excitement and curiosity when it comes to learning their baby’s gender. With modern prenatal technology offering multiple ways to predict fetal *******, many families find themselves comparing two of the most common options: ultrasound imaging and blood-based testing. Each method promises insights at different stages of pregnancy, yet their accuracy, reliability, and purpose vary in meaningful ways. Understanding these differences is essential—not only to manage expectations but also to choose the most suitable approach based on timing, medical needs, and personal preference.
In Canada, where access to advanced prenatal care is generally strong, parents are increasingly asking which option provides the clearest and earliest answer. While some hope for a definitive result before the mid-pregnancy anatomy scan, others want information rooted in medical precision. This article explores how each method works, what influences its accuracy, and how parents can determine which approach best aligns with their situation.
How Ultrasound Determines a Baby’s Gender
Ultrasound remains one of the most widely used and trusted tools for determining a baby’s gender. Unlike laboratory-based methods, ultrasound relies on real-time imaging, allowing clinicians to visually assess the development of external genitalia. In most cases, the earliest reliable window for determining fetal ******* begins around 18 to 20 weeks, when the anatomy scan provides a clear and comprehensive view of the baby’s growth. Before that point, the structures may be too small or not yet fully defined, which can reduce accuracy.
The clarity of ultrasound results depends on several practical factors. The baby’s position is one of the most important. If the fetus is curled up, facing downward, or covering the genital area with its legs, the sonographer may not be able to obtain a confident view. Maternal body composition and the amount of amniotic fluid also influence the sharpness of the images. Even with these variables, experienced sonographers often achieve high levels of accuracy when conditions are optimal.
Advances in portable imaging have further improved accessibility. Today, clinicians can perform examinations using a
handheld ultrasound device, allowing for quicker assessments in clinics, rural areas, or mobile care settings. Although these portable tools offer convenience, their accuracy still relies heavily on the user’s skill and the fetus’s position.
Ultimately, ultrasound provides a comprehensive picture of fetal development while offering gender determination as part of a broader medical assessment. Its value extends far beyond knowing whether the baby is a boy or girl, making it a core component of prenatal care across Canada.
How Blood-Based Gender Tests Work (NIPT and Other Methods)
Blood-based gender testing has gained significant popularity in recent years, largely due to its ability to detect fetal ******* earlier in pregnancy than traditional ultrasound. The most widely used method is the Non-Invasive Prenatal Test (NIPT), which analyzes fragments of cell-free fetal DNA circulating in the mother’s bloodstream. These DNA fragments originate from the placenta and can typically be detected as early as the 10th week of pregnancy. By examining the presence or absence of Y-chromosome material, laboratories can determine fetal ******* with a very high degree of accuracy.
Clinical NIPT tests performed through licensed Canadian healthcare providers are generally considered the most reliable. They undergo strict laboratory analysis and provide accuracy rates often above 99% for gender prediction. However, it is important to understand that NIPT is primarily designed to screen for chromosomal conditions such as trisomy 21, trisomy 18, and trisomy 13. Gender determination is an additional feature not the core purpose of the test.
Meanwhile, consumer-oriented at-home gender tests also exist, but their reliability varies significantly. These kits may offer early results, yet they often lack the rigorous processing standards of clinical laboratories. Factors such as contamination, insufficient fetal DNA, or improper sample handling can lead to misleading outcomes.
Even clinical blood tests have limitations. A low fetal fraction meaning an insufficient amount of fetal DNA in the sample can reduce accuracy or require a repeat test. Certain maternal conditions, high BMI, or early gestational age may also affect results.
Overall, blood-based gender testing offers an early, highly accurate, and science-backed option for families seeking answers sooner in pregnancy. Still, understanding the context, purpose, and limits of these tests ensures parents make informed decisions rather than relying solely on a single method.
Accuracy Comparison Ultrasound vs. Blood Tests
When comparing ultrasound and blood-based gender tests, accuracy is often the deciding factor for many parents. Both methods are widely used in Canada, yet they differ in timing, purpose, and reliability. Ultrasound provides a visual confirmation of fetal anatomy, meaning its accuracy is highly dependent on the baby’s position, the quality of the equipment, and the expertise of the sonographer. Under ideal circumstances—typically around the 18- to 20-week anatomy scan accuracy is generally high, but early ultrasounds are far less predictable.
Blood-based tests, especially clinical NIPT, are known for their exceptional precision. By analyzing fetal DNA directly, these tests remove many of the variables that can affect imaging. As long as the fetal fraction is adequate, NIPT can achieve accuracy rates above 99% for gender prediction. However, it is essential to remember that NIPT is still a screening test, and rare biological factors can occasionally influence results.
Which Method Is Best? Practical Recommendations for Parents
The most suitable gender prediction method depends on what parents value—whether it’s early results, medical accuracy or a more natural approach aligned with routine prenatal care. For those seeking answers early in pregnancy, clinical NIPT is often the most reliable option, offering high accuracy from week 10. However, it’s important to remember that its main purpose is screening for chromosomal conditions, with gender identification as an added feature.
Ultrasound is ideal for parents who prefer a non-invasive method that provides broader insight into fetal development. The anatomy scan not only reveals gender but also evaluates the baby’s overall health, which many families find equally important.
Some parents choose to use both methods—NIPT for early clarity and ultrasound for confirmation. Ultimately, the best choice depends on individual priorities and the type of information families feel most comfortable relying on during pregnancy.
Conclusion
Ultrasound and blood-based testing each offer reliable ways to predict a baby’s gender, yet they differ in purpose, timing, and practical benefits. Blood tests such as NIPT deliver early, highly accurate results, while ultrasound provides visual confirmation as part of a broader assessment of fetal health. Many parents find value in using both methods at different stages of pregnancy. By understanding the strengths and limitations of each option, families can make informed choices that reflect their preferences, medical needs, and expectations during this significant chapter of prenatal care.















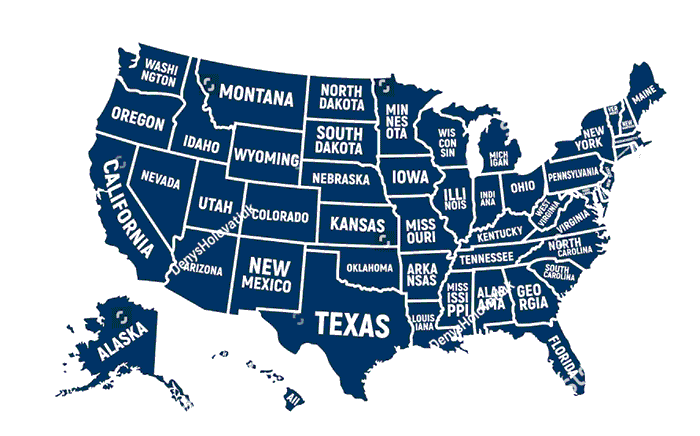 ایالت های آمریکا؛ نگاهی جامع به ساختار سیاسی و جغرافیایی ایالات متحده
ایالت های آمریکا؛ نگاهی جامع به ساختار سیاسی و جغرافیایی ایالات متحده بهترین مارک تسمه تایم ساندرو؛ مقایسه برندهای اصلی در سال ۱۴۰۴
بهترین مارک تسمه تایم ساندرو؛ مقایسه برندهای اصلی در سال ۱۴۰۴/139624430-56a75c643df78cf77294fd37.jpg) 7 کاربرد اساسی پلایی وود
7 کاربرد اساسی پلایی وود/https://www.thestar.com/content/dam/thestar/news/world/2013/09/02/devils_breath_could_be_worlds_scariest_drug/angels_trumpets.jpg) نفس شیطان: ترسناک ترین ماده مخدر دنیا!! سریال قورباغه حقیقت دارد!
نفس شیطان: ترسناک ترین ماده مخدر دنیا!! سریال قورباغه حقیقت دارد! آیفون 11 پرومکس یا سامسونگ گلکسی نوت 10 پلاس؟ | طراحی |
آیفون 11 پرومکس یا سامسونگ گلکسی نوت 10 پلاس؟ | طراحی | انواع چمن مصنوعی به همراه نکات طلایی!
انواع چمن مصنوعی به همراه نکات طلایی! آلزایمر چیست؟ علائم و روش های درمان الزایمر سالمندان
آلزایمر چیست؟ علائم و روش های درمان الزایمر سالمندان تفاوت هولوگرام و لیبل اموال
تفاوت هولوگرام و لیبل اموال